With the advancements in universal newborn hearing screening (UNHS), identifying infants with hearing loss has become relatively easy to implement. Unfortunately, how to proceed with amplification after identification is not always clear. Although there is research to support what is "best" when it comes to pediatric hearing aid fittings, many of us do not employ what has been shown to be most beneficial for our young patients. This course will address best protocols for fitting infants and young children with amplification. This paper addresses basic concepts related to the fitting of amplification to infants and young children. Topics will include the Real-Ear-to-Coupler Difference (RECD) and the prescriptive methods, namely Desired Sensation Level (DSL) and National Acoustics Laboratory NL1 (NAL-NL1).
Introduction
With the implementation of universal newborn hearing screening (UNHS) programs in the Unites States and the rapid increase in the number of states and birthing facilities conducting UNHS, the average age of identification of newborns with hearing loss over the last 20 years has decreased from approximately 30 months of age (Harrison & Roush, 1996) to approximately 6 months of age (Centers for Disease Control, 2004). Although more infants and young children are being identified at an earlier age, those children who have hearing loss and do not receive appropriate habilitation will likely fall behind their hearing peers in language, cognition, and social-emotional development. Infants who are hard of hearing or deaf and receive intervention before six months of age typically maintain language development commensurate with their cognitive abilities through 5 years of age (Yoshinaga-Itano, Sedey, Coulter, & Mehl, 1998).
Amplification may be considered the single most important intervention to help the child with hearing impairment. Amplification will, in most instances, provide the child the ability to access residual hearing so that speech and language can develop at or near age-appropriate milestones. Amplification for infants and young children will not, however, enable a child with hearing impairment to perform at a level consistent with normal-hearing peers in all situations. A realistic goal of amplification for children with hearing loss is to make speech audible at a comfortable level and provide as many acoustic cues as possible, without over-amplifying sounds, especially those that are loud.
In 2003, the American Academy of Audiology (AAA) published the Pediatric Amplification Protocol (American Academy of Audiology, 2004). It was written by a task force comprised of experts in the field of pediatric Audiology and amplification to address the significant need for guidance in this area of Audiology. It consists of 10 critical areas of pediatric amplification, which include Personnel Qualification, Candidacy, Pre-selection Issues and Procedures, Circuitry-Signal Processing, Hearing Instrument Selection/Fitting Considerations, Verification, Hearing Instrument Orientation and Training, Validation, and Follow-up and Referral. In addition, the task force addressed issues relating to appropriate equipment, experience/expertise, and the need for referral when either of these are lacking. The Pediatric Amplification Protocol will be referenced throughout this paper.
In order to organize the fitting process of amplification for infants and young children, other professionals have designed outlines (Beauchaine, 2001; Mueller and Hall, 1998). Beauchaine organizes her amplification protocol into six steps:
Assessment or identification of an infant with hearing loss consists of multiple tests as a means to cross-check test results. Otoacoustic emissions, auditory brainstem response, behavioral testing (including visual reinforcement audiometry or conditioned play audiometry), and speech detection or recognition testing are recommended; which tests are utilized will be determined based upon the child's age and developmental status. It is critical to note that click threshold data alone from ABR is not sufficient to fit amplification; alternating polarity clicks and tone bursts (500 to 4000 Hz) are essential. At the minimum, in addition to the above procedures, a complete child and family history should be taken and middle ear testing should also be performed.
After an infant or young child is identified with hearing loss, the intervention process begins. (Counseling a family with a child with a newly-identified hearing loss is beyond the scope of this paper. The reader is referred to Babies & hearing loss: A guide for families about follow-up medical care, www.perinatalweb.org/content/viw/23/41). Intervention usually begins with the making of custom earmolds. No child is too young for earmold impressions. The physical fit of earmolds is important for both comfort and retention. In addition, earmolds should be made of a soft material (vinyl is preferable) for safety as well. As children grow quickly, it is not uncommon for earmolds to need replacing at least three to four times a year, especially whenever feedback occurs at optimal settings, the fit becomes loose, or comfort issues arise. Retention devices and options include "huggies™," toupee tape, retention cords ("Critter Clips™") or headbands. Of course, counseling the parents on care and maintenance of the hearing instruments is imperative in the process of fitting amplification.
Verification/Selection
The RECD should be measured in the next step. The RECD is the "Difference in decibels, as a function of frequency, between the SPL at a specified measurement point in the ear canal and the SPL in a 2cc coupler for a specified input signal" (Pumford and Sinclair, 2001, n.p.). The RECD is used to individualize the dBHL to dBSPL transform. This is important in a population where ear canal volume and eardrum impedance greatly differ from the adult averages typically used to conduct these transforms (Scollie, Seewald, Cornelisse, & Jenstad, 1998; Seewald & Scollie, 1999). In addition, the RECD is used to adjust the electroacoustic fitting so the final output in the real ear will be correct for an individual child based on a pediatric amplification algorithm (Seewald & Scollie, 1999). This use of the measurement is especially important when real-ear aided response measures are not possible (e.g., with a very young or noisy child). With the RECD, we can convert from dBHL (insert phones or, now, ABR threshold data) to dBSPL. This is helpful when using hearing aid prescriptive methods that use the SPL-O-GRAM, such as the Desired Sensation Level (DSL) or National Acoustics Laboratory Non-Linear 1 (NAL-NL1).
The most useful application of the RECD is for the prediction of real-ear hearing aid output. RECD allows us to evaluate the difference between output in the real-ear and the 2cc coupler, so that real-ear hearing aid output (real-ear aided response or real-ear saturation response) can be measured within approximately 2 dB of target (Seewald & Scollie, 1999). Simply stated, the RECD is used to convert hearing aid performance measured in a 2cc coupler into real-ear hearing aid performance.
RECD can be performed while the infant or child is already sedated or asleep for ABR testing. For older children, it is suggested a mirror be used so the child can see what is happening. The use of Oto-ease or a Comply Wrap™ strip can be helpful (see Figure 1). Another helpful hint is to use plastic film around the probe tube and the earmold or ear tip and then insert them together (Figure 2).

Figure 1. Comply Wrap used around a hearing aid.

Figure 2. Example of probe tip attached to ear tip.
Note. From Scollie, 2006b. Available via the March, 2006 Articles Archive on www.audiologyonline.com
Insertion depth of the probe tube should be about 11 mm from the ear canal opening. It is also suggested that the patient's own earmold be used when possible, as opposed to an insert foam tip. When a new earmold is made, the RECD should be measured again. It is recommended that RECD values be obtained from both ears. It is also important to note that foam ear tips and earmold RECDs will result in very different output curves and are not universally interchangeable. If you cannot obtain the RECD for both ears, one ear is usually a good predictor for the other ear and preferable over using an "average" RECD. Age-appropriate average RECD values, however, should only be used as a last resort because of the large individual variability across RECD values in infants (Bagatto, Scollie, Seewald, Moodie, & Hoover, 2002). Using the child's measured RECD will avoid errors that occur when using an "average" value.
The procedure for RECD measurement for both ears can usually be completed in less than 10 minutes. Following are the steps needed to measure the RECD:
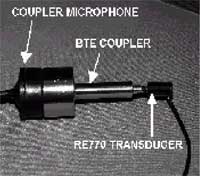
Figure 3. Measuring the real-ear response from the 2cc coupler. Note. Courtesy of Audioscan User's Manual (Audioscan, 2006b)
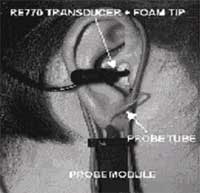
Figure 4. Measuring the Real-Ear Unaided Response with a foam tip using the Audioscan RM500. Note. Courtesy of Audioscan User's Manual (Audioscan, 2006b).
Figure 5. A RECD measurement on the Audioscan RM500. Note. Courtesy of Audioscan User's Manual (Audioscan, 2006b).
It is critical that we be able to predict hearing aid output in pediatric patients, and is thus one of the most important reasons we measure the RECD. By using the RECD, we can know the unique acoustic properties of the ear, as well as the output in dB delivered into the child's ear canal, with or without an earmold.
Utilizing the RECD has many clinical benefits. One of the most important benefits relative to this population is that the procedure requires cooperation from the child for only one measurement rather than multiple real-ear measurements. The individual prescription (DSL or NAL-NL1, etc.) can be verified in a coupler without the child present, which makes for more effective use of clinic appointment time. Additionally, hearing aid response shaping can be performed in the hearing aid test chamber under highly controlled acoustic conditions. When using the RECD instead of multiple real-ear measures, the degree of cooperation and amount of time required from the patient is greatly reduced.
Interpreting RECD data correctly is imperative as these values are directly used in the fitting process. A positive RECD value indicates the extent to which levels measured in the real ear exceed levels measured in the coupler (Figure 5). The smaller the ear canal (as is typical in younger children), the greater the sound pressure level at the tympanic membrane, and the greater the RECD. If there is a "roll-off" in the low frequencies of -1 to -5 dB, it usually indicates a slit leak, a vent larger than 1 mm, or a hardening of the earmold tubing (Figure 6). If the roll-off is large in the low frequencies (-10dB or greater), there can be a perforation of the tympanic membrane or a tympanostomy tube, as shown in Figure 7. Larger positive values in the low and mid frequencies can suggest middle ear effusion (Figure 8).
Figure 6. Roll off in the low frequencies, indicating a leakage. Note. Figure from University of Manchester: www.psych-sci.manchester.ac.uk/mchas/hearaidfitting/recdmeas.ppt#257
Figure 7. RECD indicating a perforated tympanic membrane or tympanostomy tube. Note. Figure from University of Manchester: www.psych-sci.manchester.ac.uk/mchas/hearaidfitting/recdmeas.ppt#257
Figure 8. RECD indicating middle ear effusion. Note. Figure from University of Manchester: www.psych-sci.manchester.ac.uk/mchas/hearaidfitting/recdmeas.ppt#257
Once the RECD has been measured, the hearing aid should be selected. It is possible, however, that the hearing aid has already been selected; this is acceptable as long as the audiologist has chosen amplification based on the child's degree and configuration of hearing loss, that includes appropriate circuitry and processing schemes, and meets the child's needs and the family's economic preferences (American Academy of Audiology, 2004). The goal should be to provide audibility of the amplified long-term average speech spectrum (LTASS). The following guidelines, adapted from the Minnesota Department of Health Recommended Protocol for Pediatric Amplification (2005), should always be considered when choosing amplification for infants or young children:
Assistive technology
Prescriptive Methods
The DSL prescriptive method has been used and advocated for many years in pediatric amplification fittings. The DSL method makes use of dBHL audiometric data and converts it to dBSPL at the eardrum, using the RECD measurement. As with other prescriptive formulas, the goal of DSL to select hearing aid frequency/gain characteristics that place as much of the LTASS as possible into the amplified range (Figure 9).
Figure 9. Screen shot of the Audioscan Verifit utilizing DSL, showing the amplified LTASS above threshold (Audioscan, 2006a)
A new version of DSL has recently been released. It is called DSLm[i/o] 5.0, with the "m" standing for "multi-stage" (Scollie, 2006a). As Dr. Scollie explains, DSL has always been an input/output method, but now it is multistage: expansion, linear, wide dynamic range compression (WDRC) and compression limiting. The newest version of DSL continues to focus on pediatric fittings and still uses the RECD to predict the patient's Real Ear Aided Response.
However, unlike previous versions of DSL, this version (5.0) employs two age categories: pediatrics with congenital hearing losses and adults with acquired hearing loss. The newest version prescribes more gain and output in the pediatric/congenital prescription, with the adult/acquired prescription demonstrating less gain and a slightly lower compression ratio. The overall result is that the adult targets are about 10 dB lower for mild losses and gradually move closer to the children's targets as hearing loss increases. Another improvement in the newest DSL version is that the prescriptive method takes into consideration the manner in which the child or infant was identified; specific corrections for ABR data are included in the software.
There are also new RECD normative data that take into consideration the child's age in months, as well as normative data for earmolds, as compared to foam tips. Finally, the DSLm[i/o] has four different prescriptive methods; kids in quiet, kids in noise, adults in quiet and adults in noise. Despite all these changes, the goal of the DSL method remains the same: ". to provide frequency/gain characteristics that would deliver amplified speech that was audible, comfortable and undistorted across the broadest relevant frequency range possible " (www.dslio.com/index.php?action=history) The newest version of DSL is only available at this time with the new software version 2.8 from Audioscan.
National Acoustic Laboratories (NAL) also developed a popular prescriptive method that has been used for infants, young children, and adults. The purpose of NAL-NL1 is to maximize calculated speech intelligibility and keep the overall loudness of sounds at normal or less than normal levels (National Acoustic Laboratories, 2005). The goal of their newest method, NAL-NL2, is the same. While not yet available, this new method will take into consideration "dead regions" of the cochlea. The presence of dead regions will cause reduced (or no) gain in the dead region, whereas the absence of dead regions will cause increased gain. As Dillon (2006) explains, "We have several pieces
of evidence, direct and indirect, suggesting that NAL-NL1 prescribes slightly too much gain. A review of experiments in which subjects indicated their preferred gain showed that, on average, subjects preferred a gain 4 dB lower than that prescribed by NAL-RP. Consequently, what you'll see in NAL-NL2 is a reduction of gain of about 4 dB at mid-input levels and probably a slightly bigger reduction at high input levels" (pp. 12-13). The creators of NAL-NL2 believe that the preferred gain for new versus experienced listeners is minimal, and not as worthy of further consideration. This is quite different than what the creators of DSL believe. However, the end result is similar to that of DSL: higher gain for pediatric patients.
Several research studies comparing DSL and NAL-NL1 have been conducted over the years. The most recent study described by Dillion (2006) demonstrated that the preferred gain by children was between the gain prescribed by either method (higher gain than NAL-NL1 provided, lower gain than DSL provided). In another study described by Dillion (2006) employing only adults where all were prescribed either NAL-NL1 or DSL, there was an overwhelming preference for NAL-NL1 by the subjects, driven by the DSL method being described as too loud.
There is also ongoing research studying infants who were fit randomly with either NAL-NL1 or DSL [i/o] from their first fitting. Preliminary data show no differences in performance between groups (Dillon, 2006). Results from these and numerous other studies reveal that for soft and distant sounds, the additional gain DSL provides is preferred by most. In noise, however, the lower gain in NAL sometimes is preferred.
Verification of the selected hearing aid(s) has really taken place throughout the selection and fitting processes. However, there is at least one additional issue that needs to be discussed with regard to verification of the chosen amplification. Many digital signal processing (DSP) instruments are designed to detect spectrum modulations that reflect either noise or speech inputs. Many of the test signals commonly used (e.g. pure tones) do not modulate, and thus the instrument perceives it as noise. For instruments that implement noise reduction/speech enhancement strategies, it is necessary to turn off the feature for electroacoustic verification. It is important, however, to turn it back on before your patient leaves.
"Validation of aided auditory function is a demonstration of the benefits and limitations of aided hearing abilities and begins immediately after the fitting and verification of amplification" (American Academy of Audiology, 2004, p. 15). Validation of the hearing instrument and benefit to the patient is an ongoing process, where monitoring of the instrument itself as well as the child's performance is of utmost importance. Objective as well as subjective measures are usually implemented. Objective measures, such as speech perception tests, are helpful in assessing the child's performance with the chosen instrument. Subjective questionnaires distributed to teachers and parents can also be used in the validation process. Functional gain has obvious limitations and is not the best procedure for verifying electroacoustic characteristics of the hearing aid, but can have a place in the validation process. Aided soundfield thresholds can add important information and may be used in conjunction with the real-ear measures to ensure that the child is receiving appropriate benefit from the chosen devices.
An excellent questionnaire that can be given to parents or teachers to assist in the validation process is the Children's Outcomes Worksheet (COW) (Williams, 2003). The COW is a version of the Client Oriented Scale of Improvement (COSI) (Dillon, James & Ginis, 1997) for children ages 4 to12, and provides feedback to parents and teachers about the child's performance in specific listening situations. For younger children, the Infant-Toddler Meaningful Auditory Integration Scale (IT-MAIS) (Zimmerman-Phillips, Osberger, & Robbins, 2001) is also an excellent tool.
Assessment, Selection, Verification and Validation are critical components of any pediatric amplification protocol. Each step provides the audiologist with the opportunity to assist each child with a hearing loss to the best of their ability. Regardless of which instrument you choose or which prescriptive method you employ, if all measures are completed successfully, you will be providing a child the life-changing opportunity to develop normal speech, language, social, cognitive and emotional skills.
American Academy of Audiology. (2004). Pediatric Amplification Protocol. Audiology Today, 16 (2), 46-53.
Audioscan. (2006a). Verifit test drive. Retrieved January 18, 2007, from www.audioscan.com/webpages/verifit/vf1testdrive/recdtest.htm
Audioscan. (2006b). VERIFIT® VF-1 REAL-EAR HEARING AID ANALYZER USER'S GUIDE Version 2.8. Retrieved May 1, 2007 from www.audioscan.com/resources/usersguides/Currentverifitguide.pdf
Bagatto, M.P. (2001). Optimizing your RECD measurements. The Hearing Journal, 54(9), 32, 34-36.
Bagatto, M.P., Scollie, S., Seewald, R.K., Moodie, S., & Hoover, B. (2002) Real-ear-to-coupler difference (RECD) predictions as a function of age for two coupling procedures. Journal of the American Academy of Audiology, 13(8), 407-415.
Beauchaine, K.L. (2001). An amplification protocol for infants. In R.C. Seewald & J.S. Gravel (Eds.), A Sound Foundation Through Early Amplification (pp. 105-112). Warrenville, IL: Phonak Hearing Systems.
Beauchaine, K. L., & Stelmachowicz, P. (2002). Amplification for Infants. ASHA Leader, 7, 6-7.
Centers for Disease Control. (2004). Early Hearing Detection and Intervention Programs. Retrieved January 24, 2007, from www.cdc.gov/ncbddd/ehdi/2004/DIPS_2004_final.pdf
Desired Sensation Level Method. (2005). Hearing Aid Selection. Retrieved January 20, 2007, from www.dslio.com
Desired Sensation Level Method. (2005). History of DSL. Retrieved May 4, 2007, from www.dslio.com/index.php?action=history
Dillon, H., James, A., & Ginis, J. (1997). Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. Journal of the American Academy of Audiology, 8, 27-43.
Dillon, H. (2006). What's new from NAL in hearing aid prescriptions? The Hearing Journal, 5(10), 10-16.
Harrison, M., & Roush, J. (1996). Age of suspicion, identification, and intervention for infants and young children with hearing loss: A national study. Ear & Hearing, 17(1), 55-62.
Minnesota Department of Health. (February 2005). Minnesota Newborn Hearing Screening (NHS) Program: Recommended Protocol for Newborn Hearing Screening - Revised. Retrieved January 18, 2007, from www.health.state.mn.us/divs/fh/mch/unhs/resources/amplification.html
Mueller, H.G., & Hall, J.W. (1998). Audiologist's Desk Reference, Volume 2: Audiologic Management, Rehabilitation, and Terminology. San Diego: Singular Publishing Group, Inc.
National Acoustic Laboratories. (2005). National Acoustic Laboratories. Retrieved January 10, 2007, from www.nal.gov.au/Products/NAL-NL1.htm
Perinatal Foundation. (2007). Materials and Publications. Retrieved January 18, 2007, from www.perinatalweb.org/content/viw/23/41
Pumford, J., & Sinclair, S. (2001, May 7). Real-ear measurement: Basic terminology and procedures. Audiology Online, Article 285. Retrieved April 6, 2007, from the Articles Archive on https://www.audiologyonline.com Direct URL access at www.audiologyonline.com/articles/article_detail.asp?article_id=285
RECD Measurements. (2004). Retrieved January 18, 2007, from The University of Manchester: www.psych-sci.manchester.ac.uk/mchas/hearaidfitting/recdmeas.ppt#257
Seewald, R., & Scollie, S. (1999). Infants are not average adults: Implications for audiometric testing. Hearing Journal, 52(10), 64-72.
Scollie, S., Seewald, R., Cornelisse, L., & Jenstad, L. (1998). Validity and repeatability of level-independent HL to SPL transforms. Ear and Hearing, 19(5), 407-413.
Scollie, S. (2006a). The DSL method: Improving with age. The Hearing Journal, 59(9), 10-16.
Scollie, S. (2006b, March 13). Fitting hearing aids to babies: Three things you should know. Audiology Online, Article 1545. Retrieved April 6, 2007, from the Articles Archive on https://www.audiologyonline.com Direct URL access at www.audiologyonline.com/articles/article_detail.asp?article_id=1545
Williams, C. (2003). The Children's Outcome Worksheet (COW) - an outcome measure focusing on children's needs (Ages 4-12). News from Oticon, July.
Yoshinaga-Itano, C., Sedey, A.L., Coulter, D.K. & Mehl, A.L. (1998). Language of early- and later-identified children with hearing loss. Pediatrics, 102(5), 1161-1171.
Zimmerman-Phillips, S., Robbins, A.M., & Osberger, M.J. (2001). Infant-Toddler Meaningful Auditory Integration Scale. Sylmar: Advanced Bionics Corporation.